During my working and personal life I have met people who have told me that they are on the autistic spectrum or have been diagnosed with Asperger’s syndrome. But I’ll be honest, I don’t know that much about autism or Asperger’s syndrome.
So I’m writing this Autism & Asperger’s Syndrome Series to educate myself and others.
What is Autism?
Autism spectrum disorder (ASD) is the name for a range of similar conditions, including Asperger syndrome, that affect a person’s social interaction, communication, interests and behaviour.
In children with ASD, the symptoms are present before three years of age, although a diagnosis can sometimes be made after the age of three.
It’s estimated that about 1 in every 100 people in the UK has ASD. More boys are diagnosed with the condition than girls.
(From: NHS Choices – Autism spectrum disorder (ASD), last accessed: Sunday 15th July 2018.)
What is Asperger’s Syndrome?
Asperger’s Syndrome is a Pervasive Developmental Disorder that falls within the autistic spectrum. It is a life-long condition, which affects about 1 in 200 people, more commonly in men than women. Those with Asperger’s Syndrome are usually of average or above average intelligence.
The condition is characterised by difficulties with Social Interaction, Social Communication and Flexibility of Thinking or Imagination. In addition, there may be sensory, motor and organisational difficulties.
(From: Asperger’s Syndrome Foundation – What is Asperger’s Syndrome, last accessed: Sunday 15th July 2018.)
Signs and Symptoms
The signs and symptoms include difficulties interacting with others and unusual thinking patterns. Behaviour is likely to be affected, as explained below:
Examples of Autism Spectrum Behaviours:
Communication
- Echoing words/phrases without context
- Taking an adult to the biscuit tin rather than asking or pointing
- Taking language too literally
Social Interactions
- Preference to play alone
- Difficulty relating to other people
- Not understanding other’s thoughts and emotions
Repetitive behaviours
- Hand flapping
- Toe walking
- Spinning wheels
- Lining up cars
Restrictive behaviour
- Eating only yellow food
- Insisting on walking the same route
- Only watching Thomas the Tank Engine
…
People with autism may or may not have the following:
- Exceptional attention to detail
- Sensory differences, this is most noticeable when children are over-sensitive to stimuli e.g. distress at loud noises
- Trouble with co-ordination
- Unusual eating behaviour such as only eating certain foods
- Additional learning disabilities
- A very small percentage have unusual abilities for example with music or memory
(From: Child Autism – Symptoms, last accessed: Sunday 15th July 2018.)
People with autism and Asperger’s syndrome are at higher risk of developing or have these other conditions: learning disabilities, ADHD, epilepsy, dyspraxia, dyslexia, dyscalculia, OCD, depression, anxiety, bipolar, sleeping problems, Tourette’s syndrome or other tick disorders.
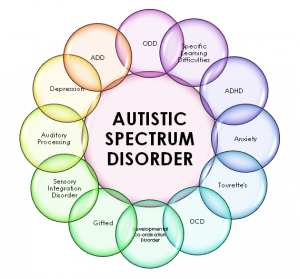
Image From & Copyright © Dream Health – Autism Spectrum Disorder, 2014.
Diagnosis
People get diagnosed with autism or Asperger’s syndrome by their GP referring them to a Specialist Team. These days people are often diagnosed as children. The specialist team usually includes a Paediatrician, a Psychologist, a Psychiatrist, a Speech & Language Therapist and a Occupational Therapist.
Treatment Approaches
As every person with autism or Asperger’s syndrome is different, the treatment for each person is different; depending on the individual’s needs. However treatment includes interventions around developing communication skills, interaction skills, the ability to imagine and traditional academic skills.
It is also useful for parents/carers and other family members to go on a parenting and autism course. This is because these courses are packed with strategies to best support a child with autism.
Parents/carers and other family members can also get peer support which will help them feel less isolated and give them opportunities to learn from others at a local support group. If there isn’t a group locally, there’s lots of message boards online.
In the next post in this Autism & Asperger’s Syndrome Series I’ll be listing useful websites around autism and Asperger’s syndrome.
Write soon,
Antony



A great introductory article on candle magic :)
Hi Sofia, Thanks for the comment. I bought that in Glastonbury and he was a real find. I bought him…
Hi! I know this was posted ages ago and so a response may be rare but my dad has been…
Hi Ruth, Thanks for the comment. He might well have been. A x
Hi! Watching video and interviews with Charlie Watt, it had me wondering if he might have had Aspergers/ been on…