This post is rather long, it wasn’t supposed to be but it just happened. So to make it easier to navigate and to read, I have split it into the following sections:
1. Nasal Polyps?
2. The Private Hospital
3. Problems with getting CT Scan Results
4. Pre-Surgery
5. The Day the Surgery was Suppose to Happen
1. Nasal Polyps?
For the past couple of months I’ve been experiencing severe swelling and pain to my nose, nasal passage and sinuses. My entire face has felt painful, including my cheek bones, jaw and teeth. My nose has been constantly congested and I’ve had to be prescribed strong painkillers from the GP – which only numb the pain, not eliminate it.
The pain I can honestly say, is the worst pain I’ve ever experienced.
I had been seeing my GP regarding these symptoms every few days, had lost count of the amount of times I’d gone to see various Doctors at my GP Surgery about the same issue. I felt like I was getting nowhere and the symptoms were only getting worse.
The symptoms became so unmanageable that I felt I had no choice but to visit to my local A&E Department. A kind Doctor there and the only one to ever look up my nose diagnosed me with nasal polyps. He said I needed to have the polyps removed by an Ear, Nose & Throat (ENT) Surgeon. He explained that the waiting list was significant, that it would take at least several months before the surgery would be completed. He explained that I would need further time off work to recovery post surgery. While I really appreciated his honesty, I could not bare to even think about being in this much pain for several months.
After this I booked another appointment at my GP surgery and requested an urgent ENT referral to my local NHS Hospital. The next available appointment was in 6 weeks time.
I discussed the situation with my mum, some friends and one of the actual named GPs at my surgery. The named GP was brilliant, it’s just such a shame that normally I can never get an appointment with him, even when I specifically request to see him. I decided I had no choice but to go for private healthcare.
2. The Private Hospital
I was initially very impressed with the private hospital. They offered me an appointment the same day I telephoned. I chose to go the next day to allow me some time to gather the required funds for the initial consultation. The next day was a Saturday, but this wasn’t a problem as they have some ENT Surgeons who routinely offer weekend appointments at no extra charge.
The hospital itself was impressive to the untrained eye. Free parking, plush waiting areas with comfortable seats and complementary self-serve hot drinks while you wait for your appointment. The friendly reception staff greeted you warmly and weren’t behind bullet proof glass. Although I noticed and appreciated these positive differences, I am not an untrained eye. I am a Registered Nurse with significant experience working in hospital settings.
On the way into the hospital, I spotted a display proudly boasting how the hospital was investing £1m in an Intensive Care Unit (ICU), which is above the level private hospitals are required to have. Let me tell you the truth about an ICU, they take several millions of pounds to set up (think machines, equipment & medicines) and several millions of pounds a year to run safely (think staff 24/7 with the correct training, knowledge and experience).
I suppose that having some sort of ICU onsite is better than them downing tools if something goes wrong during surgery and dialling 999 for an NHS ambulance to take you to an NHS hospital for care and treatment. Which believe it or not, is what some private hospitals do here in the UK. But a million pound investment is like a drop in the ocean and certainly not something to boast about.
The ENT Surgeon was and is amazing. Very experienced and knowledgeable. I really can’t fault the speed in which I got my initial or follow up consultations. You could argue that’s what I’m paying for, but I still really appreciated it. Unfortunately on the day of my initial consultation, I developed a severe bacterial nose and sinus infection (see I Didn’t Know Whether to Laugh or Cry) and turned up looking like the Elephant Man due to the swelling. The ENT Surgeon’s treatment plan was excellent and included the appropriate medications that I was able to pick up from the onsite Pharmacy.
3. Problems with getting CT Scan Results
I decided to go back to see the ENT Surgeon as soon as the infection cleared, which was exactly 1 week after my initial consultation, a Saturday again. Despite this not being the original plan, the ENT Surgeon was happy see me again. I explained and stressed the urgency of getting this health problem resolved as soon as possible due to the extreme pain and because I need to return to work as soon as possible. An urgent CT Scan was arranged for a few days later. The CT Scan was very expensive considering the small area scanned. This was were I hit my first problem with the private healthcare hospital.
I wanted to see my CT Scan after I had it. But this was not possible. I was advised to go away and fill in a Medical Records Form to request a copy of the images and report. Then I’d have to come back to the hospital once Medical Records and Legal Team had approved my request with photo ID to get a copy of the images and report. I’ll be honest, I wasn’t rude, but I was assertive. I got a form off them and completed it there and then. I gave them my photo ID to photocopy, so that I didn’t an unnecessary 60 mile round trip at a later point.
I had a further consultation with the ENT Surgeon and he diagnosed my with a perforated septum (a hole in the septum in my nose). He took a more detailed history off me. All the times (which were many) over the past few years that I had a blocked nose, I put down to developing an allergy to my cats. But they weren’t an allergy at all. Instead recurrent infections that have slowly ate away at my septum. The treatment: surgery to repair the hole. But privately it wasn’t going to be cheap.
I began ringing the Medical Records Team to chase progress of my request on a daily basis (Monday to Friday during their operating hours). I was hoping that if I could share this with my ENT Team at my local NHS and that they might consider moving me up the list as an urgent case. I repeatedly stressed the urgency of getting hold of these results to the Medical Records Team and explained that this was causing a potential delay in my care and treatment that could result in a nasal collapse. There was no sense of urgency with them and it felt like they didn’t care. At one point I began to ask to speak to someone in Management, several days in a row and was put through to an unanswered phone. I emailed them and again this went unanswered.
So I decided to email the Chief Executive and Chief Nurse of the private healthcare group that runs the hospital. Within a couple of hours of sending the email, where I had mentioned that I would be seeking legal advice if my nose collapsed (think Michael Jackson) while I was awaiting them to release the CT Scan results to me and email arrived with both the CT Scan images and report.
About an hour after that I had an Operational Manager from the hospital telephone me to see if there was anything else she could do to help me. I’m pretty sure from her tone of voice that she was asking through gritted teeth, but I had got the CT Scan results that I needed. At this point, I was very disappointed in the administration/management side of the private hospital.
I shared my CT scan results with the NHS and they were still saying the waiting list was several months long for surgery. So continuing the private healthcare was my best option at getting quick treatment.
4. Pre-Surgery
On 12/01/24 I contacted the ENT Surgeon and booked for the first available surgery date which was this Friday just gone (26/01/24). He confirmed that he’d sent the booking form in that day. On Monday just gone (22/01/24), I still hadn’t received a Pre-Op Assessment appointment or a fixed-price quote that would need to be paid before the surgery at the hospital.
I contacted the hospital and they didn’t even know that I was due to come in on Friday for the surgery. In other words: They hadn’t processed the booking form sent in by the ENT Surgeon. I had to contact him to get him to chase it. The private hospital had let itself down with failure to follow its own administrative processes. This is frustrating because with the amount of money I was due to pay them, you’d think they’d want the surgery to go ahead, as if it doesn’t they don’t get paid.
The hospital sent the fixed-price quote for the surgery the next day, Tuesday (23/01/24) and also telephoned me to arrange my Pre-Op Assessments for the following day.
Wednesday (24/01/24) – The Pre-Op Nurses were friendly, kind and a real credit to the hospital. I seemed to pass the Pre-Op Assessment, after an assessment, an ECG test and a blood sample to find out my current Diabetic HbA1c level (link goes to Diabetes UK).
For about a week leading up to the surgery, I had been struggling with episodes of severe intense pain that were so bad that it made me cry and scream in agony at the same time. This was in addition to the constant pain in my nose, face, sinuses, head, jaw and teeth I feel on a daily basis. These episodes began to affect my mental health and it had began to deteriorate. Just hold on, I said to myself. From Friday, things will start to get better, I reassured myself. There was a plan and I was doing everything I could do.
Before I go on to my experience on the day of the surgery, you’ll notice I haven’t named the private hospital or private healthcare group that operates it. That’s because I really wouldn’t recommend them to anyone. In fact I’d tell people to avoid them. I refuse to give them any free publicity or promotion by naming them here.
But in case you really want to know: Their own publicity material state they are the private healthcare hospital group of the year and the particular hospital is located near Didsbury in Manchester.
5. The Day the Surgery was Supposed to Happen
A kind friend had agreed to take me to the hospital, pick me up when I was done and take me home. I had followed every instruction given by the Pre-Op Nurses. I booked in and was taken to my private room. I saw a Nurse who asked me some questions and took my observations, including a Blood Sugar reading.
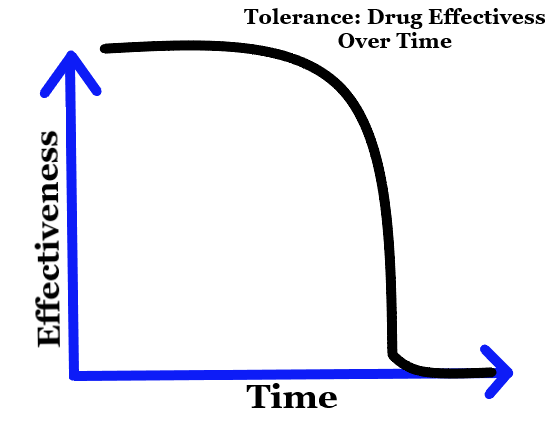
Then the Consultant Anaesthetist comes in to see me. I’ll be honest he came into the room with a bad attitude and was quite frankly rude. It took all of my self-control to speak to him respectfully and not to speak to him as he was speaking to me. He said he wasn’t prepared to anesthetise me for the surgery because my HbA1c level was too high. He stated that he felt the risk of complications were too high. I asked what it was and he said 84mmol/mol. I explained that the I was tested at the beginning of December and it was 99mmol/mol, so it is improving. I explained that I am currently checking my blood sugar as recommended and taking my medicines (including insulin) as prescribed. I explained that I am currently waiting to see a Diabetic Consultant under the care of the NHS.
I explained that I have had repeated infections in the past twelve months, which has increased my HbA1c level. I asked at what level it would need to be at in order for him to be happy for the surgery to go ahead. He said he would want a HbA1c level of 42-48mmol/mol. I explained that this is a normal HbA1c level for a non-diabetic and that this was unrealistic for me. I explained why by explaining what occurs during Type 1 Diabetes in the body and explained that my body is also insulin-resistant. I also explained the constant pain and sometimes agony I am experiencing, even on prescription only painkillers and that I don’t think that I can cope with pain for much longer. I explained that it is affecting my mental health and making me feel suicidal. He didn’t show any empathy or even acknowledge what I’d said. I explained that I have on several previous occasions had aesthetic and surgical procedures with a raised HbA1c, without any complications.
I asked what happens now. He said I couldn’t have the surgery. He started to say that if I could meet his target for my HbA1c level the surgery could be re-booked for a couple of week’s time. I explained that the HbA1c level takes months not weeks to come down and that it might not come down at all, as pain increases blood sugar levels and I’m currently in constant pain. I began to become tearful and repeated that I don’t think I could tolerate this pain for months and repeated that it is making me feel suicidal.
The Consultant Anaesthetist made his excuses and left the room. I was and I beyond devastated. I haven’t the words to explain just how severely hopeless I felt and feel. The ENT Consultant came to see me before I left. I could see he was disappointed for me. He apologised and said he there had been several discussions with the Anaesthetist, but he would not change his position. I asked: What do I do now? What’s the plan? The ENT Consultant said the only thing he could suggest is that I go back to the NHS to see if they could keep me in hospital for a week before the surgery to reduce my HbA1c level before doing the surgery. The ENT Consultant said that he would speak to my local NHS hospital to see if he could help to arrange this. He reassured me that he wasn’t going to just abandon me. He was extremely kind and I thanked him for this.
I messaged my friend, he came to pick me up and we left. My mind and emotions were and are all over the place. I really don’t know what to do next. The constant pain makes it difficult for me to even think straight. I feel completely out of control and there doesn’t seem to be anything I can do to stop the pain by getting the underlying cause treated. I feel low and it feels hopeless. My quality of life is the poorest its ever been. I feel physically, mentally, emotionally and spiritually broken. Last night, I was so low, I even considered ringing the Samaritans.
But I have to remind myself of a couple of things. First, where there is life, there is hope. Second, the only certainly in life is change. The pain. How I feel now. Both will change.
Take Care,
Antony