In recent years the pharmacological principle of prescribing and administering the minimum dose of medication to get the desired effect has become common place in medicine. Despite not being a Doctor or Nurse Prescriber I have come to believe that this approach is fundamentally wrong. In this post I explain why.
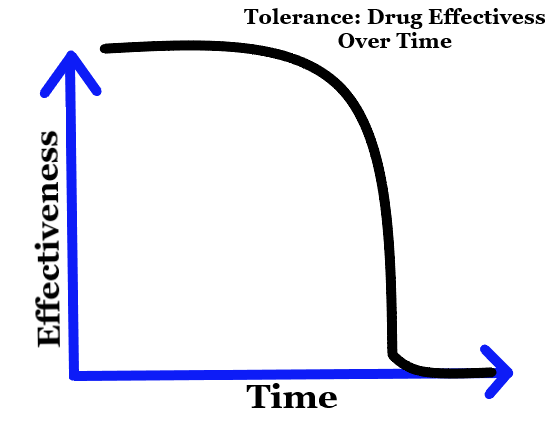
Let me explain why the theory and practice has become so popular. It has lots of benefits. It helps prevent patients being overdosed on medications, minimises the likelihood and severity of side effects; can prevent or reduce the risk of patients becoming tolerant to medications and microbes from developing drug resistance (such as antibiotic resistance).
These benefits all sound good, so lets looks at the risks and why I believe the risks outweigh the benefits – put simply why I think this approach is wrong.
The biggest risk is that patients get under-dosed, leaving them in pain or suffering due to Doctors and Nurses being too cautious. Another risk is that Doctors and Nurses are always looking to reduce doses at medication reviews. This could be physically, mentally and emotionally harmful to the patient. Some may argue that pathways are in place to prevent under-dosing and harm. But pathways don’t always account for the complexity of the individual patients.
Here are some examples of when this theory of giving the minimum amount of medication to get the desired effect doesn’t work:
- A patient brakes their arm and has the bone sticking out. They are understandably in a lot of acute pain. However a pathway, Doctor or Nurse may choose to start them on paracetamol and work up to stronger painkillers. In this case the patient is likely to need Morphine, which is at the top of the pain management pathway. This may result in several hours (or more) of severe pain.
- A patient with chronic back pain attends a Pain Service for medication review. After the initial assessment, the Doctor or Nurse decides to lower doses of medications despite the patient saying that they’re struggling with the pain. They refer to Physiotherapy – a good decision, but still reduce the doses of medications. This leads to anxiety, possible depression and more physical pain.
- An elderly patient has a urine infection and type 2 diabetes. After several GP visits due to constantly needing the toilet, she gets antibiotics. However they are of the lowest dose, indicated by a urine infection pathway. The patient has to return to the GP to get a higher dose. During this time her blood sugars are high, leading to even more urination, the risk of dehydration and other associated complications of having a high blood sugar over a prolonged period of time.
- A patient with mental illness such as bipolar isn’t put on high enough doses of antipsychotics and/or antidepressants. They are given the dose that is as little as possible and it is not increased despite the patient asking for this. This means that the patient has continual relapses and repeated admissions to mental health wards.
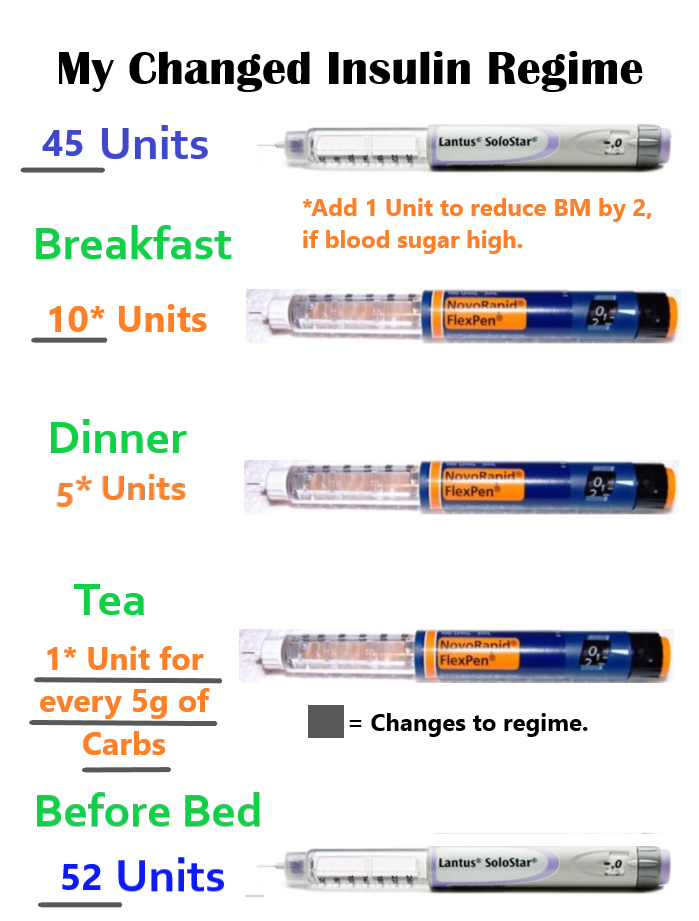
I try to avoid writing about things that could cause controversy. But my recent 15 day stay in a mental health ward and experience with community mental health services has left me having being given less than the standard doses advised in the BNF on two mood stabilisers. I believe that standard doses of medications exist for a reason. These are levels of medication that experienced clinicians through research have found to be effective.
I now face an uphill struggle and a battle to get medications I need increasing increased due to this theory. This is why I believe it is fundamentally wrong. Because of the risks of under-dosing and causing harm. I’m sure I’m not the only one affected by this principle, it is no doubt many others across the country and Western world.
Write soon,
Antony