There aren’t a lot of famous people who’ve been open about their HIV status. This is not surprising given the historic stigma associated with HIV. In the 1980s there was a real lack of information about HIV/AIDS, this led to myths and a lot of fear. There were also no treatments. This was a public information broadcast back in 1986, and it really shows how little we knew about HIV/AIDS and what a diagnosis meant (death):
But there are some brave people who have been open about being HIV positive.
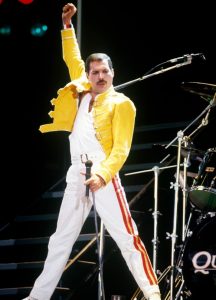 Freddie Mercry [Deceased], Singer. Image from & Copyright © People.com. |
1. Freddie Mercury Perhaps the most famous person to be open about their HIV positive diagnosis was the legendary Freddie Mercury. He opened up about his HIV positive diagnosis the day before his death. What is fascinating about Freddie Mercury is that he has been remembered for the way he lived, not the way he died. He is remembered for his work: writing songs, singing them and fabulous performances. If I could have tea with anyone from any time, living or dead it would probably be Freddie Mercury. As a fellow creative soul (albetit not in the same field) I’d love to know where he got his inspiration. How he came up with his ideas. How he managed to find the magic melodies and be ahead of his time, yet timeless at the same time. Freddie Mercury gave very few interviews, so I guess I’ll never know the answers to these questions. |
 Gareth Thomas, Retired Professional Rugby Player. Image from & Copyright © Wikipedia. |
2. Gareth Thomas Gareth Thomas is a Retired Professional Rugby Player from Wales, UK. Gareth Thomas disclosed his HIV status as being positive, yet also being undetectable and untransmittable earlier this year. His HIV status really shows how far treatment for HIV has come. Once a death sentence, it is now a treatable condition. Many people who are HIV positive can now have the same life span as those who are HIV negative. Prior to this Gareth Thomas is the first major sportsman to come out as gay in Rugby, which he did so in 2009. Rugby is a very masculine sport, so he should be commended for being honest and open about his sexuality. |
 Andrew Bell, Singer. Image from and Copyright © The Info NG. |
3. Andrew Bell Andrew Bell is the lead singer in the band Erasure. In 2004 he disclosed his HIV positive status to the public. Since Andrew Bell’s disclosure he has been involved with a number of charities raising funds for HIV research and projects. This includes work with National AIDS Trust (NAT). |
 Charlie Sheen, Actor. Image from and Copyright © GQ. |
4. Charlie Sheen Charlie Sheen is an Actor with a checkered past. His past according to several sources includes violence, alcohol and substance misuse and being very sexually promiscuous. It is the latter of these behaviours that probably led to Charlie Sheen being diagnosed as HIV positive. In 2015 Charlie Sheen disclosed his HIV status in an interview. In the same interview he reported that he had spent approximately $10 million to keep extortionists quiet about his HIV status. |
 Christopher Smith, Retired Politician. Image from and Copyright © The Info NG. |
5. Christopher Smith Christopher Smith is a Retired Politician in the UK. I didn’t know that he even existed before doing research for this blog post. He is one of the unsung heroes in the LGBT community. Christopher Smith was the first gay male Politician to come out, coming out as gay in 1984. He has severed in several Governments and has undoubtedly influenced people’s views about people who are LGBT. He has probably supported legislation for LGBT rights and promoted a more inclusive and equal culture. |
I am aware that there are no women on this list. I couldn’t find a single famous female who has been open about their HIV positive diagnosis. If you know one, please leave a comment below and let me know.
A HIV positive diagnosis used to be like a death sentence, but today it isn’t. Treatments for HIV positive have never been better and have led to people with HIV being found to be undetectable and untransmitable. Want to know more about HIV? Learn more here.
Write soon,
Antony